by Dr Mairead Murphy, Honorary Research Fellow, Centre for Academic Primary Care, University of Bristol and Evaluation Lead, South West Academic Health Science Network
“I think everyone’s been in the situation where they go to a doctor to talk about something that they find hard to talk about or they might find it difficult to voice their concerns.”
“I just couldn’t get a word in edgewise, sometimes you find you’ve just arrived and the GP is writing the prescription you know?”
These are some of the things patients said to us when we interviewed them for the Consultation Open and Close (COAC) study. Patients felt that, in the 10-minute consultation, particularly when it was by telephone, the GP did not always have time to get to the root of their problems.
This is not new or surprising. The 10-minute GP consultation is the shortest in Europe. Telephone consultations are becoming the norm and these are known to be more transactional and pose increased risk if overused. Patients sometimes feel interrupted by GPs or that they didn’t get their main problem resolved.
At the same time, the public opinion of general practice is worsening while GPs are working harder than they have ever done, burnt-out and leaving the profession, and having to deal with ever more complex problems.
While there is no silver bullet to solve these problems, we found something that might help.
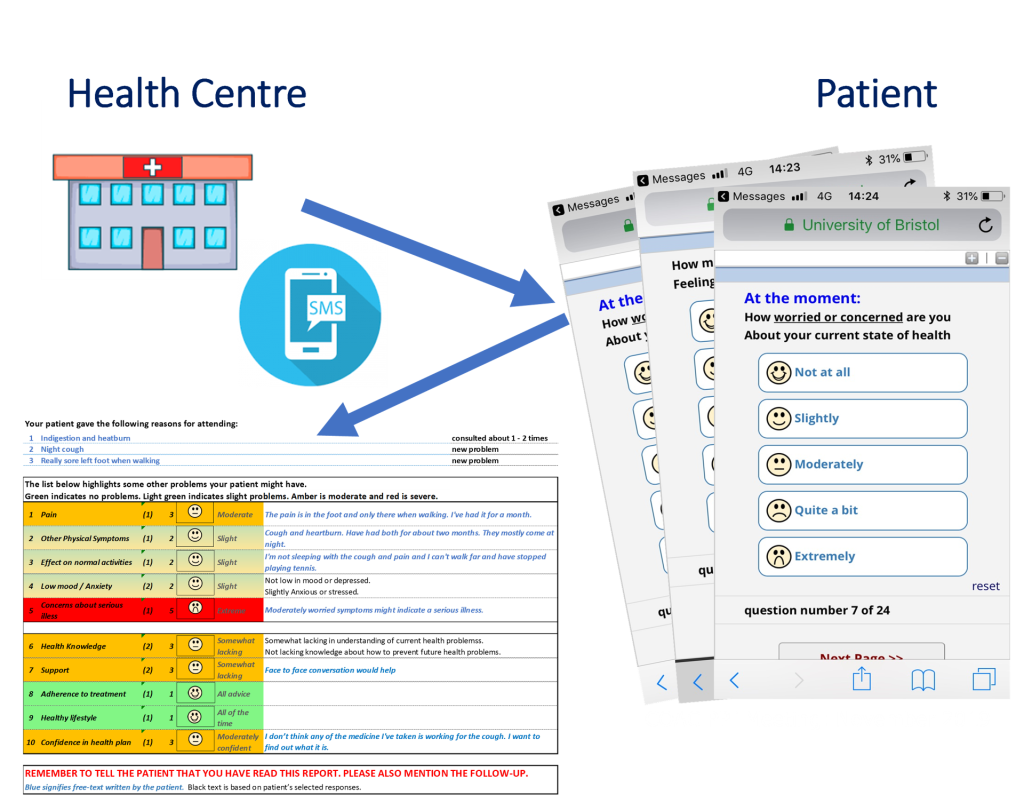
In the COAC study, we developed, tested and piloted a new online form for patients to complete before a GP consultation. Unlike an online triage form, this was designed for patients to complete once they had secured a consultation. Patients receive an SMS just before their consultation and complete the form on computer or phone. A summary of their responses then gets attached to the patient record for the GP to review before the consultation.
The form invites patients to provide more information on common concerns, like pain, physical symptoms, low mood, whether they are worried about their health and whether they needed help managing. It uses a colour-coded fixed format, so GPs quickly got used to reading it and it took up very little time:
“It was really easy for me to read, I scanned it in 20-30 seconds.”
“It worked well in terms of […] getting to the heart of the issue earlier on that you probably would have done otherwise in the consultation.”
Patients felt more listened to and understood after completing the form:
“I felt that she was able to read what I’d put prior to actually speaking to me [on phone] so she understood better.”
“It’s a bugbear of mine every time I leave the doctors, you can’t really get it all out. But her knowing it already helped.”
The COAC study also looked at helping at the end of the consultation. As well as not being able to express their problems at the beginning, some patients said they found it hard to remember what was said at the end of a complex consultation.
We developed a clinical protocol and template which GPs can use to create a summary for patients at the end of the consultation. GPs used this for patients where they have given them multiple follow-up steps, or important safety-netting advice and they thought the patient might not remember the advice or properly process it.
The patients who were given this found it really helpful:
“She gave me quite a lot of information over the telephone, had it not been in a report I probably wouldn’t have remembered all of it.”
“If it’s written down and I can refer back to it, then that’s far easier. And with my father, it means we can take it home and then discuss it when he’s less tired and able to take it in.”
“You can follow up and you can challenge it … it does set a little target for both parties in a way which at the moment is quite useful.”
The two forms need further development before they can be implemented, but are useful prototypes illustrating what can be done to improve the opening and close of consultations, with benefits for both patients and GPs.
Sharing our findings and next steps
We have published three papers describing the development of the forms in the National Institute for Health and Care Research (NIHR) Open Journals:
- The person-based development and realist evaluation of a pre-consultation form for GP consultations
- The person-based development and realist evaluation of a summary report for GP consultations
- The consultation open and close study: A feasibility study of a complex intervention
We are currently working with Bristol, North Somerset and South Gloucestershire Integrated Care Board (BNSSG ICB) to implement the summary report forms in general practice in the region. The findings from our work on the pre-consultation form are being used to inform a social health insurance scheme to collection patient-reported outcome measures routinely in Austria.
For more information, visit the COAC Study website.
Disclaimer
This research was funded by the National Institute for Health and Care Research (NIHR). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department for Health and Social Care.